A dog or cat may suffer from discospondylitis, an infection of the intervertebral disc.
What is discospondylitis?
The term “discospondylitis” refers to an infection of the discs between the vertebrae (intervertebral discs) caused by bacteria or fungi. This infection can occur in any area of the spinal column, and it can occur at multiple sites. It is also known as spondylitis, intervertebral disc infection, and vertebral osteomyelitis. A dog is more likely to suffer from discospondylitis than a cat.
What causes discospondylitis?
There are several ways in which a bacterial or fungal infection may reach the intervertebral discs.
- The most common method is through the bloodstream. It is possible for bacteria to enter the bloodstream and travel to the disc area from chronic skin infections, urinary tract infections, prostate infections, etc.
- Directly through punctures or bite wounds near the spine, or through procedures or surgeries near the spine.
- As a result of foreign bodies migrating through the area near the spine.
Bacteria:
Bacteria such as Staphylococcus, Streptococcus, Escherichia coli, and Brucella spp. are commonly isolated organisms. Pseudomonas, Proteus, Pasteurella, Corynebacterium, and Actinomyces spp. are sometimes found. Reproductive problems may occur with Brucella infections and this carries a risk to people. There are reports of pets infected with Bordetella spp., Erysipelothrix rhusiopathiae, and Salmonella spp.
Fungi:
Fungal organisms that can cause Discospondylitis include Aspergillus, Blastomyces, Histoplasma, Coccidioides spp., and occasionally Paceilomyces. In Europe, infection with Rasamsonia argillacea has been reported. A single case of infection with Westerdykella spp. has also been reported in a German shepherd dog. Fungal infections can be more difficult to diagnose than bacterial infections, so looking for enlarged lymph nodes, lung or eye lesions, and fungal organisms in the urine can help.
Other Agents:
Protothecosis, a disease caused by a type of green alga, has been associated with discospondylitis.
What are the signs of discospondylitis?
There is a gradual onset and progressive nature to the signs. A variety of signs may be experienced at the beginning, including spinal pain, stiffness, and unsteady walking. The most common sign is spinal pain, which is manifested by spontaneous yelping, even if animals are not touched. The weakness is usually mild, unless the infection enters the vertebral canal. A pet’s condition can worsen if they do not receive appropriate treatment, as fractures of the vertebra can lead to paralysis. Muscles adjacent to the spine may atrophy (degenerate); this is most likely the result of nerve damage or myositis (inflammation of the muscles).
Infections can cause spinal cord compression by granulation tissue, bony changes, or fractures and dislocations (luxations). It may be necessary to perform surgery to stabilise vertebral fractures or dislocations.
In rare cases, the infection may lead to meningitis, meningomyelitis, or a spinal abscess.
How do I diagnose discospondylitis?
It is important to consider further imaging if there is evidence of spinal pain with the clinical signs mentioned above. Various imaging modalities (CT scans or MRI), urinalysis (and culture), bacterial cultures, serology, and cerebrospinal fluid analysis may be necessary for the diagnosis.
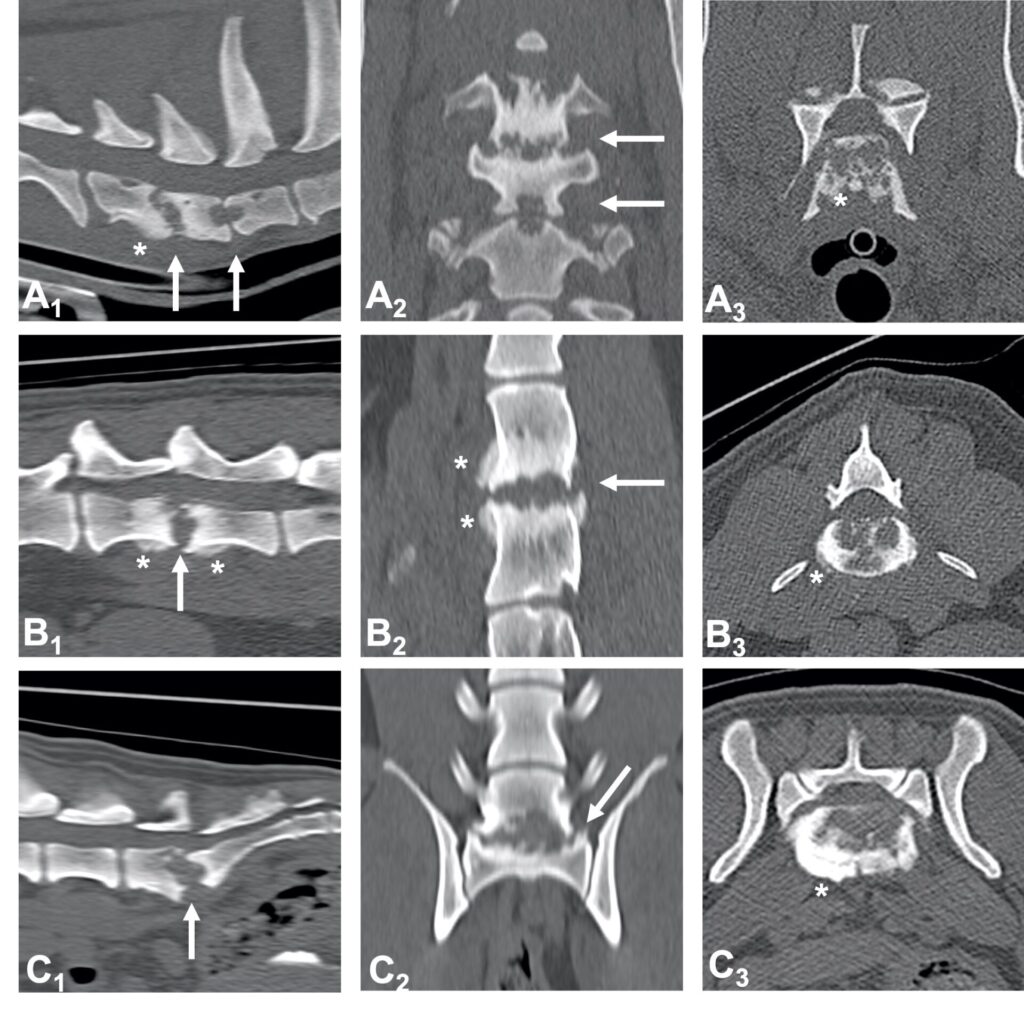
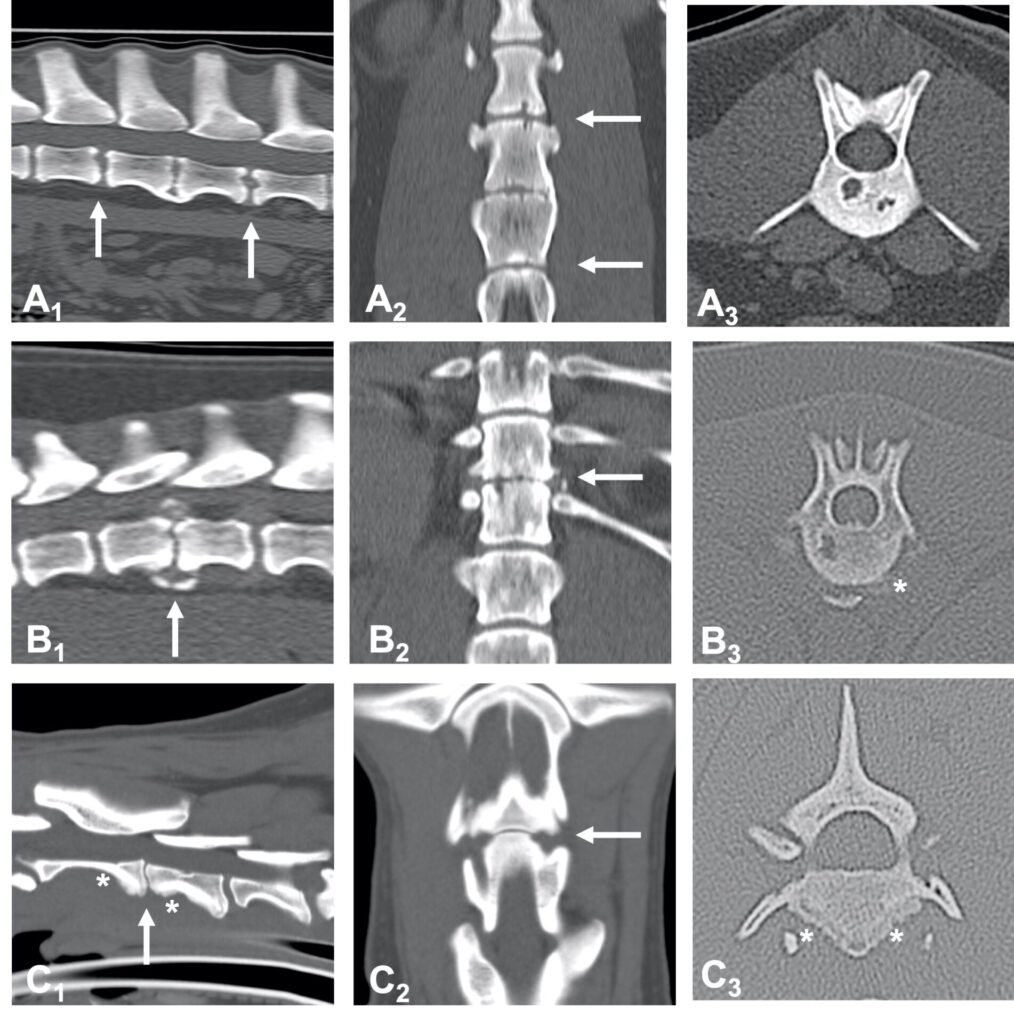
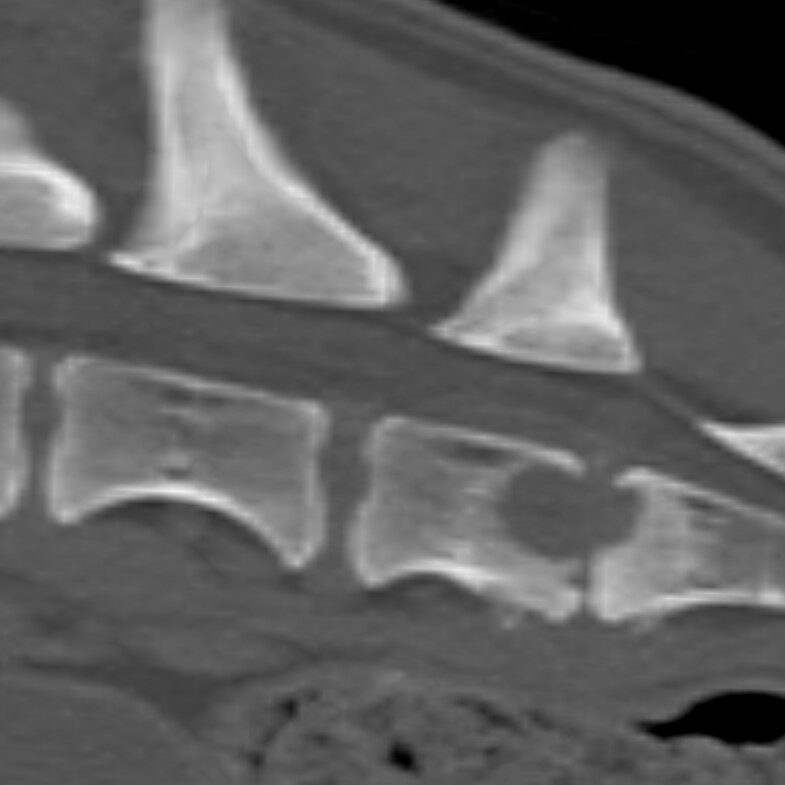
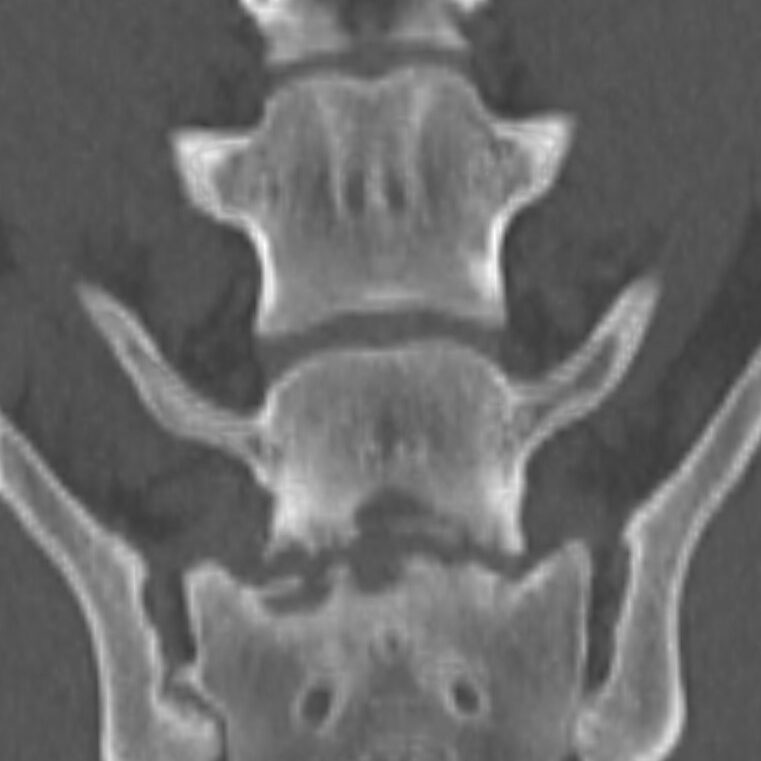
A radiograph of the spine will typically reveal damage to the vertebrae adjacent to the affected disc. The spine can become deformed and undergo bone changes as a result of chronic conditions. Radiographs may not show changes for 3-6 weeks after clinical signs begin, so if the first radiographs are normal, but the clinical signs are progressing, it is sensible to repeat them some time later.
When a typical lesion is detected, radiographs of the entire spine are recommended since some pets have multiple lesions. When a disc is infected, it degenerates and destroys the ends of adjacent vertebrae. There is evidence that these degenerative changes may weaken the vertebral column and make it more susceptible to pathologic fractures, which are caused by infection rather than trauma. As part of the healing process, the body may attempt to bridge the damaged area with bone, which may encroach on the spinal cord and nerve roots, resulting in further complications.
Imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) are more sensitive than plain radiography, particularly when it comes to detecting the problem early on.
It may be possible to identify the organism(s) that caused the infection by culturing urine, blood, spinal fluid, or other infected tissues. To obtain the most accurate results, it is recommended that a culture of the infected disc space be conducted. In order to obtain the best sample, it may be necessary to perform fluoroscopically guided fine needle aspiration. The infected areas of the spine should be harvested and cultured if spinal surgery is necessary.
Testing for Brucellosis serology (looking for current and previous infections in the blood) is recommended. Brucellosis is one of the possible causes of discospondylitis and can be transmitted to humans. There is a tendency for this to occur only in dogs who have travelled abroad. There is a particular risk associated with dogs re-homed from Eastern Europe.
The analysis of spinal fluid (CSF) is necessary in animals with neurological signs. As well as culturing the CSF, routine cytology, cell count, and protein determination are performed.
Can discospondylitis be treated?
An antibiotic course that is specific to the organism that is causing the infection is required for treatment. Ideally, the antibiotic should be selected based on the results of culture and sensitivity tests performed on the infected disc. In the absence of disc culture, antibiotics will be selected based on the results of culture results from urine, blood, or other areas that have been infected.
It is possible that antibiotic treatment will be required for many months. Recurrence of the disease or persistence of signs may result from the abrupt discontinuation of antibiotic therapy, ineffective antibiotics, or if corticosteroids, or other immunosuppressive drugs are used. If clinical signs do not improve while the pet is taking antibiotics, you may decide to repeat the disc culture.
The treatment of Brucella infections is not curable, and the risk posed to humans is so great that euthanasia is often recommended.
Some cases of fungal discospondylitis may be treated with antifungal drugs, particularly itraconazole.
When a lesion does not respond to treatment or has persistent draining tracts that indicate foreign body migration, you may suggest surgical exploration. Decompressive surgery and/or stabilisation may be considered if evidence of spinal cord compression is found on myelography or MRI, or if severe, progressive neurological problems occur. When spinal instability is a significant complication of the operation, surgical stabilisation may be beneficial.
There may only be a need for pain medications for a few days if antibiotics prove to be effective.
Will a pet recover from discospondylitis?
Prognosis for recovery is variable and depends, to some degree, on the cause of the discospondylitis.